Every now and then, discussion amongst clinicians turns to the hypothetical of “what if you were stranded on a desert island?” and then leads into fierce debate on emergency drugs, preferred contents of a doctors bag or various airway devices.
Of course all of this is hypothetical – not many of us are going to be stranded, Lost-style, on a desert island and forced to manage an airway. In an ideal world we’d all work in a well-stocked theatre or ED with a variety of equipment to manage the difficult airway…
But many of us do work in areas where choice of equipment is needfully limited – such as in the prehospital and retrieval environment, or in rural & remote areas. Limitations may be imposed by cost, by size and shape, by weight or by need to fulfil various functions.
To my mind equipment for airway management in such areas should be not just readily available, but allow a suite of options, be affordable and offer advantages in both routine and emergency situations. Standard difficult airway plans usually revolve around Plans A, B, C & D
- Plan A – Primary intubation strategy (eg: direct or videolaryngoscopy)
- Plan B – Alternative intubation strategy (eg: videolaryngoscopy or intubation through LMA as conduit)
- Plan C – Maintenance of ventilation (eg: bag-mask ventilation, supraglottic LMA ventilation or to allow awakening (the resumption of spontaneous ventilation requires no residual paralysis)
- Plan D- Rescue techniques for the “can’t intubate, can’t ventilate” scenario ie: emergency surgical airway
[of course, plans may be adapted to suit patient eg: initial plan for an awake fibreoptic, with back up plan in case of deterioration involving double-set up of ‘one look’ laryngoscopy, then rapid progression to a primary surgical airway in a case of massive supraglottic oedema, etc]
Much has been written elsewhere about DL vs VL and Emergency Surgical Airways. I won’t rehash them here, but instead point interested people towards EMcrit here and here respectively…. but what of the humble LMA in our airway plannng?
Available LMAs
For many years, the Classic LMA (cLMA) has been the stalwart of rescue ventilation. It is a familiar tool to many – indeed can be placed by trained volunteers such as ambulance officers in rural and remote areas. But the design has been improved; many second-generation LMAs offer the following :
- integral bite-block
- gastric drainage channel
- ability to allow higher ventilation pressures
Many ambulance services have considered switching from the Classic LMA to the LMA Supreme (sLMA), as it has both bite-block, gastric drainage and allows higher pressures than the cLMA. However, like the cLMA, the sLMA is a lousy conduit for fibreoptic intubation.
Other devices exist, for example the Ambu AuraGain – an LMA which has bite block, gastric drainage and is specifically designed to function as a conduit for fibreoptic intubation via LMA. The iGel (pictured above) is in a similar mould, although like the Ambu does not allow BLIND passage of an ETT for intubation.
“the ability to place an ETT through an LMA, whether blind or with a fibreoptic scope, is a powerful combination for a back-up airway device”
Of course for placement of an ETT blindly through the LMA, there is the FastTrach intubating LMA. This has been around for a while, and allows blind intubation through the hyperangulated channel. Success rates for blind intubation through the device are good, reportedly at 81-100% – success can be improved to 95-100% with a flexible fibreoptic scope using the FastTrach as a conduit to facilitate intubation.
Flexible fibreoptic intubation is not a skill available in many austere environments, nor necessarily a skill of many emergency physicians…but a malleable fibreoptic stylet is both relatively easy to learn and can be a cheap addition to a difficult airway kit. But the hyperangulated channel of the Fastrach won’t accommodate a malleable stylet!
Other problems of the Fastrach are that it has no gastric drainage port, which seems to be a major downfall in a product designed as a rescue device in an emergency.
It is also notoriously difficult to remove the LMA over the ETT once in situ – best advice is to leave the LMA-ETT complex in situ once successfully placed, and perform a careful removal in a place of safety such as the operating theatre with multiple backups. There have been cases of the airway being lost during removal of the LMA over ETT, most notably as part of the cascade of catastrophes in the infamous Gordon Ewing’s or ‘exploding scrotum’ case…
Moreover the Fastrach is a bulky device and primarily used as a backup LMA specifically for placement of an ETT. It does not come in paediatric sizes. It would NOT be your primary LMA for rescue ventilation or use in a prehospital pack, although some use it as a backup backup LMA…
The Desert Island Airway
The IDEAL device for use as part of an airway kit in an austere environment (the ‘desert island airway’) should serve as a backup for laryngoscopy, allow gastric drainage, have an integral bite block, be relatively compact and able to serve as both primary and backup LMA, and finally to allow both BLIND and FIBREOPTIC intubation.
The AirQ is such a device. I think it’s the bees knees for my difficult airway kit – and I am not alone (EMcrit covered this device ages ago – it has seen some improvements since)
I had the unexpected good fortune to run into Dr Daniel Cook last week at Adelaide airport; Daniel was over in Adelaide for the ANZCA Anaesthetic Conference and headed stateside..whilst I was on y way to Melbourne to instruct on the rather excellent “critically ill airway” (CIA) course with a star-studded Australian faculty.
There are several AirQ devices in the family – I am a growing fan of the Air-Qsp blocker model. There’s no pilot balloon, the LMA cuff self-pressurises. Most importantly it comes in a variety of sizes and is both cheap and small enough to serve as primary rescue LMA AND as an intubating LMA.
If I had to chose one LMA only, then this device ticks boxes for both prehospital service or use on the airway trolley in an austere environment (ED resus, ICU, ward, rural etc). It has advantages of being
- cheap
- of a compact size for storgae in pack or trolley
- range of sizes
- allows simple ventilation as an LMA
- allows placement of an orogastric tube to drain stomach
- has an integral bite block
- allows intubation either blind, or via fibreoptic device (both via expensive flexible scope or cheaper malleable stylet)
It’s also a lot less fiddly to remove an LMA over the ETT when placed via the AirQ than the Fastrach and has some nice touches – the anaesthetic circuit connector is detachable but is held in place via a plastic retainer (it’s very easy to drop these connectors when under stress or hands slick with saliva, blood or lube)…the packaging also contains a bronchoscope adaptor, allowing ongoing ventilation if decide to place an ETT by flexible fibreoptic scope – a little detail, but an absolute boon as prevents “needless faffing around looking for a bronch adaptor” in a time of crisis!

Staged Airway Management for Transition from Prehospital to ED Care
But I think the REAL game-changer is that use of such a device allows a staged approach to airway management. In the past, I’ve seen ambulance services place a classic LMA for eg: OOHCA – typically this is where intubation is either not an option (volunteers or paramedics) or has failed despite being within their skill set (difficult intubation).
Leaving aside the fact that such the classic LMA device do not accommodate high ventilation pressures, their downfall is that that cannot function as a conduit for an ETT nor do they have a bite block or gastric drainage.
So the OOHCA survivor may arrive in ED Resus, with a soiled airway, biting down on the cLMA and now generating negative pressure pulmonary oedema….and the resus may grind to a halt as the ED team take out the LMA and perform laryngoscopy to place an ETT. We would see the same with the Supreme LMA (although both gastric drainage and bite block are significant advantages)…but due to the narrow diameter of the channel, the sLMA still needs to be removed if an ETT is to be placed. The iGel and Ambu AuraGain do allow passage of an ETT…but only with a flexible fibreoptic scope – rarely available immediately in ED. So blind intubation is probably best in the ED via an LMA placed earlier in the prehospital arena…
The Fastrach allows blind intubation, but is expensive and bulky, so unlikely to be used as the primary back up airway in a prehospital service. Gastric drainage is not possible unless one deflates the cuff to allow tube passage…it’s a good device…but too expensive and bulky to be used as primary LMA, in my opinion.
To my mind the Air-Q LMA actually allows a staged approach to airway and progression from prehospital to hospital or as ascend the airway skill gradient. Specifically, it is
- small enough and cheap enough to be available across a prehospital service or rural hospital network
- allow gastric drainage and high ventilation pressures, with an integral bite block
- can be placed by relatively inexperienced staff
- then allows an ETT can be placed blindly by success rate improved with either a malleable fibreoptic stylet or a flexible fibreoptic scope in the ED whilst resus continues…
I’ve never worked in an ED where flexible fibreoptic is immediately available (perhaps it should!)…but the reality is that flexible fibreoptic is a skill that needs regular skills maintenance – whereas the use of a malleable fibreoptic stylet (such as the Levitan FPS) is pretty straightforward and can be easily used through the AirQ…
So – if I could only have one LMA, I’d go for the Air-Q. Admittedly the blind intubation rate isn’t as good as Fastrach (although this can be improved by extension of the neck and application external laryngeal manipulation) – but it is small, affordable, comes in a range of sizes and allows a staged progression in airway management without interruption – indeed it appears designed for this.
On this basis, it is my recommendation for a single LMA with variety of uses in prehospital and rural environments where flexible fibreoptic scopes are not available.
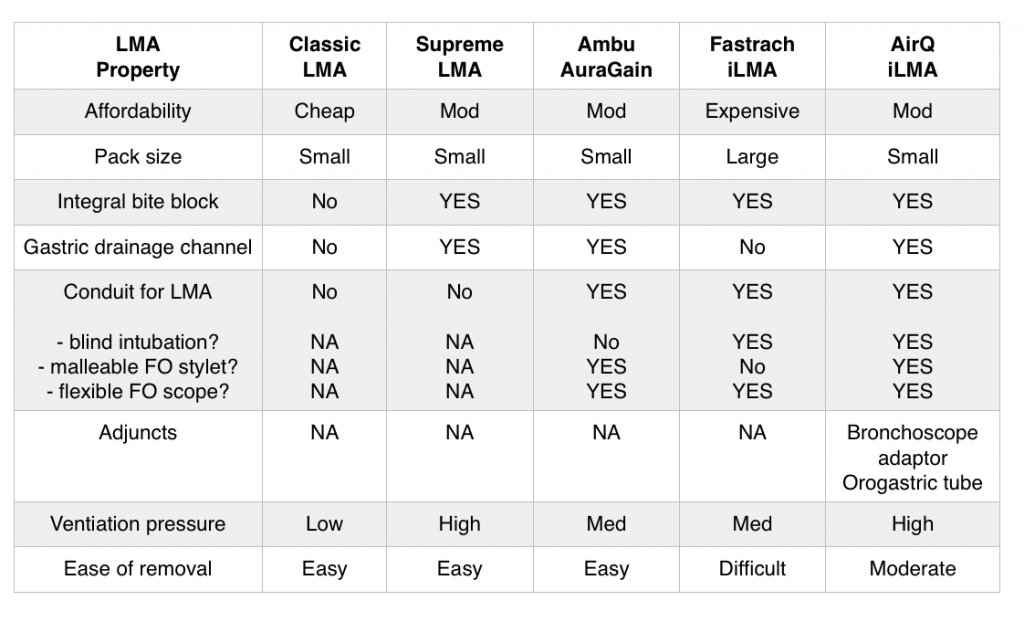
The table below summarises pros and cons of various LMAs discussed above.
I should add that the AirQ comes in paediatric sizes – unlike the Fastrach…
Watch a quick video of the Air-Q from the inventor Dan Cook here
https://www.youtube.com/watch?v=E0a1KYwfDk0
Jim DuCanto demonstrates intubation using a malleable stylet through the AirQ here:
References :
Blind versus Fibreoptic Laryngoscopic Intubation through Air Q Laryngeal Mask Airway El-Ganzouri et al 2011 https://kidocs.org/wp-content/uploads/2015/05/Blind-vs-FO-intubation-through-AirQ.pdf
Comparison of blind tracheal intubation through the intubating laryngeal mask airway (Fastrach) and the Air-Q Karim et al 2011 https://kidocs.org/wp-content/uploads/2015/05/Karim_et_al-2011-Anaesthesia.pdf
Fatal Accident Inquiry into the Death of Gordon Ewing available at http://www.scotcourts.gov.uk/opinions/2010FAI15.html
Supraglottic airways – the history and current state of prehospital airway adjuncts. Ostermayer & Gaushe-Hill 2014 https://kidocs.org/wp-content/uploads/2015/05/Current-state-of-supraglottic-airways.pdf
Tips and tricks to improve the success rate of blind tracheal intubation through the Air-Q versus the intubating laryngeal mask airway Fastrach. Badawi et al 2013 https://kidocs.org/wp-content/uploads/2015/05/Tips-n-tricks-to-increase-success-of-blind-intubation-w-AirQ.pdf
See also REVIEW OF AIR-Q from EMcrit here http://emcrit.org/airway/cookgas-air-q/




thanks Tim
Can I ask if you have ever used an AirQ in prehospital care?
Yeah mate, I have been carrying them in my pack for a couple of years now – just updated to the new AirQsp model (without pilot cuff).
Used for two OOCHAs – easy to insert (opted to use instead of the ambo classic), then drop down an orogastric. Blindly intubated through one, used FO for the other.
They pack small (about size of classic-supreme) and have a wider range of size than the Fastrachs etc.
I remain equivocal on the ‘blocker’ component (the supplied orogastric tube has a balloon to occlude the oesophagus)…I have one for each size of AirQ copackaged with the LMA – advantage is that this way I remember to pass an OGT, something I have sometimes forgotten in past.
My main caveat with AirQ is that success rate for blind intubation is less than Fastrach…something like 77% vs 91%….can be improved via neck extension and BURP/ELM….but the former not terribly useful in trauma.
But…on balance…small packaging, variable size and versatility from blind-FO stylet to FO intubation plus cognitive forcing of OGT makes it a winner for me…
iGel might be an option although blind ETT through it is not great…rates of intubation iGel vs AirQ with FO (flex) are about same (at least from a paeds study I saw)
Do you want me to flick some up your way? I’ve found a new supplier in SA.
tim
thanks
thought so.
I got a bunch of the AirQs a few years ago when DuCanto suggested them. Thats when we had the Levitan FPS and it works well with an optical stylet. Blind ETI via the AirQ is not much joy.
IN my prehospital XP and the prehospital airway literature its hard to go past the Fastrach. Lots of European EMS literature on it. AirQ has almost no published EMS literature on it. Its a good SGA no doubt. Just hard to say if its better than the others in its league.
The iGel as you know is used by a number of prehospital services overseas and in Oz.
LMA Supreme is replacing the Classic LMA here in Queensland Ambulance.
I think SAAS went with the LMA Supreme too.
I believe its best to have a SGA that you can easily insert with little training and then ventilate without doing to much fine tuning maneuvers. Whether you can intubate via the SGA is a luxury and should not be the deciding factor in acquiring a SGA for emergency kit.
I am also mindful we should choose airway gear not just for personal use but for colleagues who are coming to work as locums or relievers.
So if your local/statewide ambulance service is going with Xbrand SGA then I think it pays to be consistent cause thats what they will be bringing patients in on. Our staff should be conversant with that device at the very least.
Yeah mate – agree completely!
Classic LMA is still the SGA of choice here in Ambulance. Retrieval carry one Fastrach (size 4 if I recall correctly). Dunno if it’s ever been used!
There have been mutterings about switching to another device for several years….and there are a plethora of devices out there. Supreme and iGel favoured interstate…
So – it’s open to debate. Supreme is a nice device – gastric drain, bite block, easy insertion. Can’t place an ETT through it though….and the point I am trying to make is that devices such as iGel, AirQ allow a staged airway…place prehospital, then segue into an ETT as resus continues, without grinding to a halt to perform DL/VL…but the iGel doesnt allow blind, AirQ does.
Fastrach great – but limited by cost, bulkiness and available size range.
Many factors to consider. We could go around in circles forever debating. How many Fastrachs do you carry in prehospital pack? Enough sizes for all patients?
One device to do the lot would seem sensible. I am not sure we’re there yet – but AirQ close
Certainly not been used much in Australasia…seems to be popular overseas. Do you advocate concordance between States and Territories? Between ambulance, retrieval and ED in terms of kit carried? That would be something….
Meanwhile : Supraglottic Airways: The History and Current State of Prehospital Airway Adjuncts
Ostermayer, Daniel G. ; Gausche-Hill, Marianne :2014
Prehospital Emergency Care, 2014, Vol.18(1), p.106-115 covers pros/cons nicely – advantage is range of sizes inc paeds.
The lack of published studies on use of AirQ in prehospital is surely one ripe for study….similar criticisms made re : iGel, but we all know who uses it!
Fair point re: locums. EVERYONE knows hot to whack in a classic. But I am surprised how many EM trainees (and some anaes) who have never had hands on with iGel, Fastrach and other devices…
Learning how to use a fastrach for first time in anger is not sensible. It’s easy enough to place..but you need to know the Chandy manouevre etc to maximise ET placement. And as for taking it off over the ETT….a world of pain!
Keep it simple. But if we are going to move on from classic (33 years old this year) then we need to consider ALL options… and then standardise and train to them
So far, evolutions have included :
cLMA to sLMA +/- Fastrach
cLMA to iGel +/- flexible scope
I can see problems with training and skills maintenance for both of these (fastrach issues alluded to above, and flexible FO kit few and far between in ED, plus hard to maintain skills)
My suggestion would be to consider
cLMA to Air-Q and keep it simple that way. With training (not hard) plus FO of choice if you insist…
But many choices. Whats YOUR desert island airway?
(pls dont say combitube)
hahahaha
we carry the 3 sizes of Fastrach. Its not perfect but I know it has rescued and intubated quite a number of difficult airways in prehospital care in my neck of the woods.
It takes practice though and the evidence suggests at least 25 successful uses before provider is reasonably proficient with it.
iGel is a dead simple device and comes in all sizes.
Supreme is also dead simple and comes in all sizes.
the AirQ is simple but it gets a bit complicated when you have to pass that blocker..not as straightforward as a SGA with a built in gastric channel.
Fastrach as a simple SGA is not bad but it has no gastric channel and only comes in 3 sizes.
You havent mentioned the King LTDS which is ubiquitous in USA. If you are going to recommend a SGA universally its hard if you dont consider what everyone else is doing.
I dont think for now we can make any strong recommendations about prehospital SGA apart from saying what we would like the ideal one to be.
The closest that fits the bill is iGel in my opinion.
it doesnt require air inflation so no need to worry about air transport issues. It comes in all sizes.
You can intubate via it. It has a built in gastric channel that diverts crap away from larynx area.
its fairly cheap.
there are few prehospital studies at the moment but more than the AirQ.
problems are that they weigh more than the other SGAs, they dont seal as well so can have a leak.
but as an overall best fit for prehospital needs, they are a good choice. GSA HEMS have gone with them and they put a lot of thought into their prehospital airway kit.
Disagree
Glad though to hear that you carry three sizes of Fastrach – that seems sensible and offers more choice than just carrying the one. Impressed that you can fit ’em into packs…but then again, you’ve got large aircraft 😉
I LIKE the iGel – small, easy to insert, gastric drainage. But the REAL strength of the device is as a conduit for fibreoptic intubation…and that needs both availability of FO and the skills to use it. I would think that is why some use it – for both use in trauma AND for passage of ETT in the difficult (obese, septic etc) secondary retrieval of patients from a rural facility…
AirQsp no longer has a need for cuff insufflation. It’s also easy to insert, has gastric drain etc…but allows blind, FO (stylet or flex) intubation. Cheaper than Fastrach. Not as bulky as Fastrach and so serves as both primary and rescue device.
Minh, if you dont feel blind intubation is necessary in a SGA, then why do you carry the Fastrach? Genuinely curious!
It will be interesting to see how experience evolves. No one device (yet) does it all – hence the ‘desert island’ airway tag line. I like the versatility of the AirQ and it’s easy to use…
They all have strengths…and weaknesses. Maybe the AirQ needs a design change to put a gastric drain into cuff and obviate the separate channel? That would work…
As for King LTDS – never tried one, not going to. They may be popular in the States – but then again, so are guns. Readers can see more of the King device here: http://www.kingsystems.com/medical-devices-supplies-products/airway-management/supraglottic-airways/disposable-supraglottic/
Looks like a sex toy to me….
SAAS still using the classic LMA. Was talk years ago of moving to LMA supreme but no movement.
When I completed my last ARC ALS course we played with classic LMA, LMA supreme and I-Gel.
For the infrequent user (non intubator) eg. RN, volly ambo, industrial paramedic, military paramedic the i-gel was very popular with the group. Less steps to insertion (less to remember or go wrong in a crisis) and the I-Gel “resus pack” that contained everything you need in one blister pack was kinda cool.
https://www.youtube.com/watch?v=ijAeVvgh7sg
Hi, I just found your blog, as a Vet Nurse previously, hospital admin worker currently, and hopefuly paramedic or nursing student…
This is a super interesting article, from my perspective of one day progressing my animal knowledge up to human level. Sterilising up to 20 cats in a few hours at a busy shelter, somewhat like a production line of sedated and clipped belly up kitties, the best assistave technology we had for intubating was a straight coat hanger inside the ET tube for better “poking” during annoying laryngospasms.
I am excited to see the possibilities for my future 🙂
Thanks for writing, and I will be going back through your posts!
Pingback: DAS 2015: Ditch the FastTrach? - KI Doc