I had the opportunity to speak to Mr Mark Wilson – a consultant Neurosurgeon and HEMS doctor in London, with a background including NASA, Everest Base Camp, rural medicine and significant input into medicine in the developing world.
Mark and I were at University College Hospital in London many moons ago. As times have moved on, so have our respective careers. According to information from the St Mary’s Hospital (Imperial College) website :
Mark underwent self imposed prolonged training, as an anaesthetist and a GP, before his neurosurgical career, but even now likes to maintain a broad medical interest. He has worked extensively overseas (India, Nepal, South Africa, as a GP in Australia, researcher for NASA and as an expedition doctor on Arctic and Everest expeditions). He wrote The Medics Guide to Work and Electives Around the World and runs www.medicstravel.org. His research is mainly into the brain in hypoxia (using it as an injury model) in humans.
I believe Mark even did a stint as Dr Mike Cadogan’s wedding photographer! Small world…
You can see his impressive CV here..and be sure to check out his talks (freely available, just credit appropriately).
Now I don’t know how Mark’s career went so badly wrong, but thank my lucky stars that my own career path at least has lead to the life of a simple country doctor in rural & remote Australia (TFIC).
Joking aside, there are common themes for Mark’s work as a neurosurgeon and pre-hospital specialist and that of the rural & remote doctor from which we can learn. And Mark was gracious enough to say that he wishes he was working as a rural doctor in Oz! So we hooked up today to chat about neurosurgical issues and the bush – you can watch the VODCAST below.
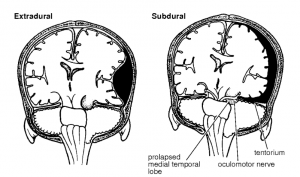
One of the classic ‘brown trousers’ scenarios in medicine is that of the seriously head-injured patient with an extra-axial haemorrhage (subdural or extradural) – the resultant compression of the brain by expanding haematoma causes brain injury and death…a mechanism that is amenable to targeted placement of a burr hole. Put simply, placing a hole in the skull allows the drainage of blood.
This is not a new concept – indeed skull trephination has been with us from Neolithic times onwards – with bone trephination used as primitive emergency surgery to remove shattered bone and blood clots typical for weapons such as slings and clubs. trephination is shown in Hieronymous Bosch’s work (below)
In 2012, Cliff Reid published on ‘life & limb’ saving procedures that should be within the remit of any Emergency Physician (and hence with which rural doctors need to be au fait). Similarly I heard Brian Burns speak on ‘Always Carry A Scalpel’ at SMACC2013 – but neither mentioned drainage of extra-axial haematoma as a core skill for ED or PHEC docs.
This is a shame as the principle is the same as other limb/life saving procedures such as finger thoracostomy, surgical airway, thoracotomy, lateral canthotomy etc – make a hole and relieve or stop the bleeding. Not a terribly complex procedure – in fact, according to comedy duo Mitchell & Webb “it’s not exactly brain surgery!”.
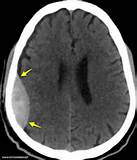
Of course the preference is to transfer such patients to a dedicated neurotrauma facility. But every now and then, especially in this large brown land, there are reports of bush doctors having to perform emergency burr holes / craniotomy to save a life. Indeed there are some reports that outcomes may be better by general surgeons in the bush than by transfer and treat approaches, due to the worsening of prognosis with delay – which can be significant in rural Australia.
Not to be gung ho about this – the preference is very much that the procedure is done by a neurosurgeon, with CT confirmation of the sire of bleeding….but every now and then it does need to be performed in outback Australia. Dr Jeff Taylor in Naracoorte, SA had to do this as did Dr Rob Carson in Maryborough, Vic also – in the latter case using a hand held drill form the hospital maintenance shed! I’ve been involved with one in rural NSW a few years back when locumming in the bush – scary to get started, but not so hard once you get going! A bit like a surgical airway…
So – have YOU got a Hudson brace, perforator drill bit and a burr hole bit in your hospital?
Better still a drill bit with a clutch mechanism as suggested by Mark and colleagues? And do you know how to use the kit?
Who is YOUR local neurosurgeon in a crisis and can you get hold of them quickly?
REFERENCES
Mitchell & Webb Brain Surgery video
Guide from the excellent austere environment guide “Primary Surgery Vol 2” on extra-axial haematoma’s and how to perform the surgery (extradural and subdural bleeds, both extra-axial)
Account of Dr Rob Carson in Maryborough using an electric drill in rural Victora
http://www.squidoo.com/Dr-Rob-Carson-Maryborough
and a similar account of Dr Jeff Taylor in Naracoorte doing the same in rural South Australia at http://www.abc.net.au/news/2004-06-08/boy-saved-as-gp-gets-surgery-tips-via-phone/1988972
Rural doctors should be aware of The Canadian Journal of Rural Practice and the excellent paper on “The Occasional Burr Hole”. The advice ‘if you are in a hurry, just read the bold type’ is classic Canadian understatement of this ‘how to do it’ guide…
For a more up-to-date guide, see Mark’s paper “Emergency burr holes: how to do it” – which emphasises the need for a clutched drill bit to avoid ‘plunge into brain’.
You may also be interested in Mark’s websites on Medics Travel and General Info inc CV etc
There’s also a section on “Teach yourself brain surgery” !

I like diagram “on passage of time” from http://www.primary-surgery.org/ps/vol2/html/sect0203.html
Pingback: Breaking out of your comfort zone | Nomadic GP
Pingback: The LITFL Review 103 - Life in the Fast Lane medical education blog
Pingback: Rural Team Entry for SimWars - KI Doc
Pingback: Clinical Governance Day 9th April 2014 | Greater Sydney Area HEMS
Pingback: Are you a Good Samaritan? - KI Doc
Thanks for the nice video. You mentioned that the extradural hematoma might be in one of several places and presumably one might not hit it with the first hole.
1) Would you make a dural cut in the first hole if you did hit the hematoma. (The burr hole isn’t so good anyway for the SDH as you mention. And we are presuming that we have a clinical hx and physical to support an extradural bleed.)
2) Would you proceed to make a second (and third) hole if the first does not pan out and where would you elect to make the 2nd and 3rd holes?