I’ve just been reading the latest Clinical Communique from the Victorian Institute of Forensic Medicine – stoked to see fellow FOAMed enthusiast Gerard Fennessey contribute, along with a reference to a paper written by Casey Parker (BroomeDocs) and myself on the value of FOAMed for rural clinicians. There’s also expert commentary from Ass. Prof Matt Hooper on retrieval services. These clinical communiques are excellent resources and a great source of tacit knowledge sharing. Check them out here
All of which has made me think about the issue of audit in rural practice. It’s very easy to ‘point the bone’ to failings in rural practice. Of course highlighting failings is important – but all too often systems seems geared more towards punishment, rather than gaining a true understanding of causative factors. And this is where audit (part of clinical governance) becomes relevant.
Clinical governance is really important. One of the (many) things I’ve learned from the prehospital environment is how clinical governance is essential to driving quality improvement. At SA Ambulance-MedSTAR (South Australia’s retrieval service), cases were audited every week which has the potential to drive quality improvement. As Hooper says in regard to retrieval services
“clinical governance, audit and educational activities should be multidisciplinary such that referral and receiving teams and the retrieval service are able to share learning outcomes….
…It is only when this occurs that the outcome for individuals disadvantaged by the need for retrieval are improved irrespective of gradients in the level of care available”
The problem of rural audit
Things in rural South Australian hospital are a little different to the finely-honed mechanism of a retrieval service. Many hospitals are staffed by visiting medical officers who work on a ‘fee for service’ basis. Some of the larger ones have salaried medical officers, but most are on a VMO basis – and are hence attend only to see hospital cases – and depart as soon as care is completed. Participation in hospital audit is far down the list compared to the pressures of running their own practice and providing an oncall service to the hospital.
Yet one of the hardest thing that rural doctors do it manage critically ill patients – such work is often required to be done with inadequate equipment and of course is performed relatively infrequently. It’s stressful and of course a potential for mistakes with adverse patient outcomes. Of course the running of the hospital itself and the training of nursing/ancillary staff is the responsibility of Country Health SA. The nursing staff across rural hospitals are, generally, of a good standard – with mandatory training and skills maintenance dictated by Country Health SA. But how about the doctors?
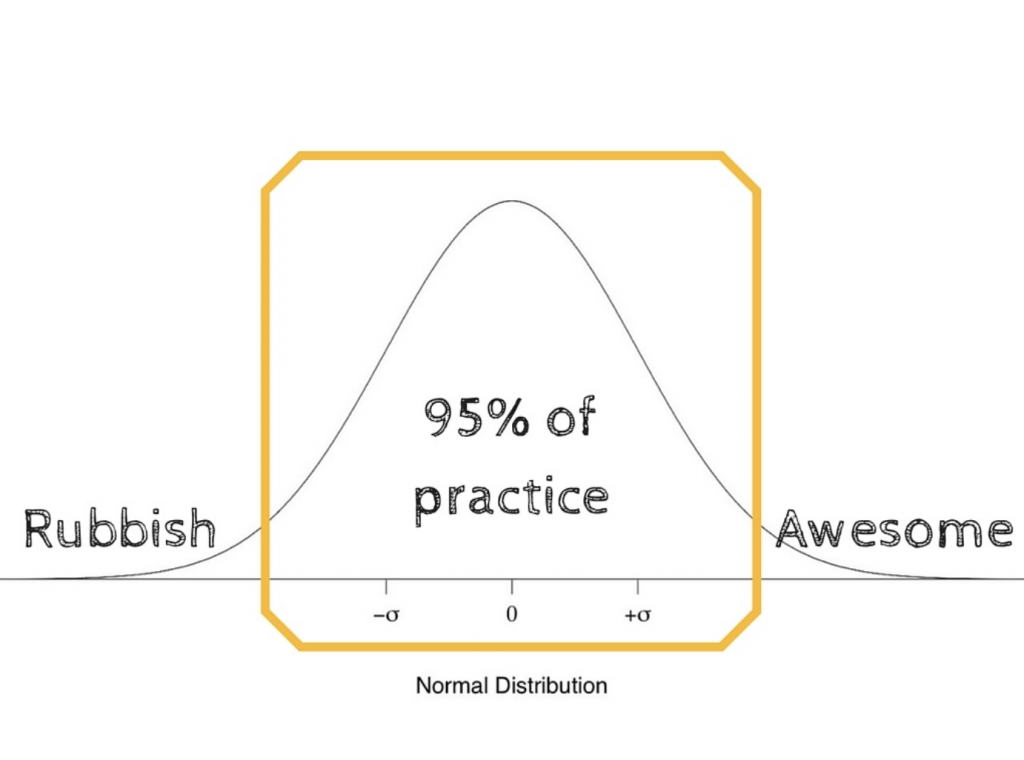
Well, some rural doctors do this sort of work very well indeed. Most are average. Some don’t do so well, understandably deskilled by the relative infrequency of such events and the paucity of equipment I am interested in how to make this better – whether through increasing access to appropriate equipment, training through in situ sim, upskilling opportunities or through reflective practice. The development of appropriate guidelines designed specifically for rural practice is best driven by audit of such cases (what works in a tertiary centre may not work so well in a rural environment- viz many massive transfusion protocols).
“The surviving sedation guidelines 2015 collaborative project is a good example of rural guideline development, taking the best evidence and applying to this environment to assist practice in an inherently high-risk clinical situation. Safe sedation and management of the soiled airway is something we practiced as sim in the RDASA Rural Docs Masterclass”
But here’s the problem – it can be hard to give feedback on such cases to team members. The retrieval service is busy and may not have time to report back. In turn the rural clinicians involved have often gone home or disappeared to clinic. Worse they may not be receptive to feedback unless delivered sensitively. Moreover, such feedback may be confined to patient outcomes, and ignore the nuances of non-technical factors in the management of critical illness. In addition, the feedback may be given to an individual clinician – but there’s not necessarily an opportunity to feedback to the team as a whole.
It’s true that many times the team members train separately – for example, upskilling courses purely for doctors, in-hospital training delivered solely for nurses. This is inevitable when scant heed is paid by organisations to the importance of human factors and the benefits of in situ team training and regular audit.
So – I am increasingly interested in the concept of feedback from all members of the resus team – as part of audit and to help drive quality improvement. Rather than look upon this as ‘finding fault’ it’s more about ‘finding a remedy’. Is this part of the solution?
Debrief – as a routine?
The concept of debrief is not new – it’s almost de rigeur after a critical incident, a cardiac arrest or a significant event (paediatric resus etc).. these are times when emotions may be raw due to the impact of the resuscitation and debrief is seen as a good thing to help individual team members make sense of the events.
But should debrief be routine after any critical illness requiring retrieval? Perhaps not in larger centres – but I think the answer has to be resounding “YES!” for small rural hospitals where managing critical illness is relatively infrequent and there is much scope for learning and improvement.
Such debrief needs to gather input from all team members in a non-judgmental manner, allowing exploration of technical and non-technical aspects as part of a commitment to quality improvement. Allowing time for all members of the team to highlight areas for improvement can generate meaningful and shared objectives for change.
Feedback and debrief can also allow positive reinforcement of practices and behaviours that worked well – rather than debrief descend into nit-picking over trivia, there’s a chance to reflect on what worked well and to praise individuals. The corollary is that causative factors in ‘what didnt work well‘ can be explored and hopefully addressed. This may be problems with communication (most often), with equipment, with clinical skills or knowledge.
There’s no doubt in my mind that the model of private VMO and salaried rural hospital staff doesn’t work well for regular team training nor audit, because such activities are unpaid extras for the VMOs – unless authorised by the hospital. This in turn leads to a disconnect, presenting a wasted opportunity for quality improvement.
“The team that trains together will improve together”
Moreover, there may not be an organisational imperative to seek feedback on such cases. I recall a comedy moment in recent years where one senior Health manager (with overriding responsibilities for one aspect of rural health) assured me that there was “no need for audit of emergency cases; we already get told what to do when the Coroner gives a report”.
So – how to overcome this?
The hot debrief
The hot debrief – immediate post event discussion amongst team members – is a good chance to drive quality improvement once the critically ill patient has left the rural hospital. Advantages are that team members are immediately available and can, if the appropriate culture exists, have a quick group huddle and talk about what went well/what could be improved.
Of course such efforts may be sabotaged if there are other imperatives – more patients to see, a messy resus bay to clean, the chance to grab something to eat….or the fact that patient outcomes are unknown. Hot debrief is a valuable tool, but can omit the ‘big picture’ of events before arrival and after levaing the rural facility.
Routine audit
I’ve been asking various people in Country Health SA for the routine audit of critical patients in rural hospitals for some time….of course it’s invaluable to have the input of the retrieval service (and this often happens).
Rather than wait passively for feedback, I believe that an extra dimension to local quality Improvement can be driven by rural hospitals using a structured tool. Feedback can be given by all members of team, whether lead clinician, nursing team member, volunteer ambulance officers, ancillary staff etc … and gives an opportunity for reflective practice once further information on the case is available
“In sim, we debrief after every case – and yet we don’t after a real emergency”
Encouraging the routine (but of course voluntary) use of feedback forms post a retrieval or resus allows chance to examine both technical and nontechnical aspects of care with a view to driving quality improvement. It requires a culture of openness, honesty and free of fear of retribution. Audit of cases is not a ‘test’ – but an opportunity to drive quality care.
Here’s one I’ve been playing with on KI – RURAL AUDIT & FEEDBACK FORM.
It has received some good feedback from colleagues interstate and I’d be keen for further feedback from readers on how this form could be improved for rural practice.
Practice elsewhere
As stated above, the retrieval service SA (MedSTAR) already do audit of each and every case and do a bloody good job of it. There model is one to aspire to. Similarly many rural anaesthetic practices (interstate at least) have regular audits and teleconferences to discuss interesting cases or ‘near misses’. This is a good thing – although as far as I know there is no involvement of rural hospitals in the National ANZ Airway registry – a wonderful initiative that has really driven change in the practice of emergency department intubation.
Wouldn’t it be awesome to have a robust system of proactive clinical governance, lead by rural clinicians, involving all involved staff – with a view to incremental improvements in quality?

Currently, it seems that SA Health has no robust audit of emergency cases in rural hospitals unless there is reporting of a critical incident or a finding from the Coroner. To my naive mind, such audit and reflective practice involving the whole team should be routine and part of our culture. In an ideal world, I’d love it if
- rural hospitals routinely audited emergency cases, especially those requiring retrieval or unusual levels of input (equipment staffing etc)
- senior clinicians in the receiving facility were able to feedback dispoisition, as well as referring clinicians making it a habit to enquire after every case ‘sent to the big hospital’
- it was easier for the busy retrieval service to ‘close the loop’
In addition to clinical feedback, meaningful audit should explore issues with communication, equipment and team dynamics.
Perhaps many of you are already routinely auditing your emergency and resus cases? If so, how are you doing it? Ad hoc? Structured? Multidisciplinary? Involving ambos, ancillary staff, nurses, doctors, admin?
I would be really interested in what is happening elsewhere in Australia – or overseas – for audit of critical care in rural locations, by rural clinicians.
RURAL AUDIT FEEDBACK FORM
References
ANZ Airway Registry – http://airwayregistry.org.au
Couper K & Perkins G (2013) Debriefing after resuscitation Curr Opin Crit Care. 2013 Jun;19(3):188-94. doi: 10.1097/MCC.0b013e32835f58aa. http://www.ncbi.nlm.nih.gov/pubmed/23426138
Fogg T et al (2012) Prospective observational study of the practice of endotracheal intubation in the emergency department of a tertiary hospital in Sydney, Australia Emergency Medicine Australasia, 2012, Vol.24(6), pp.617-624
Fogg T (2015) et al Airway Registry: Closing The Audit Loop http://airwayregistry.org.au/acem-2104-rnsh-final.pdf
Leeuwenburg T. (2012) Access to difficult airway equipment and training for rural GP-anaesthetists in Australia: results of a 2012 survey Rural and Remote Health 12: 2127. (Online) 2012 Available: http://www.rrh.org.au http://www.rrh.org.au/publishedarticles/article_print_2127.pdf
Leeuwenburg T & Parker C (2015) Free open access medical education can help rural clinicians deliver ‘quality care, out there’ Rural and Remote Health 15: 3185. (Online) 2015 http://www.rrh.org.au/publishedarticles/article_print_3185.pdf
May N (2013) It’s Good to Talk – Debrief in the Emergency Department StEmlyns Blog http://stemlynsblog.org/good-to-talk-debrief-in-the-emergency-department/
Surviving Sedation Guidelines 2015 – see guidelines as a PDF at http://kidocs.org/wp-content/uploads/2015/05/SSG2015v6.pdf – also blogpost via BroomeDocs and podcast here http://content.blubrry.com/prehospitalpodcast/PHARM-2015-05-12-119.mp3
Victorian Institute of Forensic Medicine – Clinical Communiqué – December 14, 2015 Volume 2 Issue 4 December 2015
In Victoria, as you know, retrieval is coordinated by Adult Retrieval Victoria. We have a robust system of feedback. Once we have retrieved a patient we endeavour to contact the receiving hospital within a couple of days to find out how the patient is doing, find out the diagnosis etc. We then contact the donating hospital to provide some feedback, both on the patients condition and regarding the retrieval process. One of the challenges is contacting the clinician involved and so we often rely on nursing staff to pass on any information.
Thanks Andy – same here in SA; MedSTAR retrieval do a good job – often difficult for them to track down the referring clinician! But of course the good rural docs always followup the next day
I think the real bang for buck is not so much the clinical denouement – but exploring the nuance around debriefing the rural team (usually combined of VMOs and resident nursing staff) – who have little opportunity to train together in sim nor debrief on elements of human factors influence in success of the resus…
It’s not just about what happened to the patient – it’s about how well (or not) things worked prior to the arrival of the transport service. Was there good teamwork? Was equipment available and did everyone know how to work it? How was communication? Did we have ready access to protocols to help guide us? Could we do better?
It’s more about the need for rural teams to conduct audit and reflect on own practice to improve outcomes…
I have just taken over the ‘transfers out’ case cohort of our M&M here at Ballarat from the beginning of 2016. I’ve downloaded your form and I’ll take your comments and suggestions on board. I’ll keep you posted as to our progress.
Steve