End-tidal CO2 is increasingly becoming used outside of the Operating Theatre and it is prudent for the rural doctor to have an appreciation of what it is, how to measure it, when to measure it and it’s utility in common scenarios.
“you get A, B & C in a single squiggly line”
Casey Parker, BroomeDocs.com
It is my belief that ETCO2 should be used not just in intubated patients, but as a valuable adjunct for procedural sedation, for monitoring patients ‘at risk’ and to help guide resuscitation.
What is end-tidal CO2?
Unlike plants, we breath in oxygen and exhale carbon dioxide – we can measure this as ‘end-tidal CO2’ (ETCO2). ETCO2 represents the partial pressure or maximal concentration of CO2 at the end of exhalation. The principle determinants of ETCO2 are:
(1) alveolar ventilation,
(2) pulmonary perfusion (cardiac output)
(3) CO2 production (and elimination)
How can I measure it?
We can measure ETCO2 in several ways
(i) colorimetric
Devices such as the Easy-Cap or Pedi-Cap are designed to confirm the presence or absence of expired CO2 – a pH detector (metacresol purple on filter paper) detects pH shifts and changes to the colour yellow in the presence of expired CO2.


colour change from purple to yellow indicates presence of CO2 > 2%
(ii) waveform capnography – during BMV or mechanical ventilation
A sample line is placed as a sidestream to the breathing circuit (usually via the HME filter at intersection of endotracheal tube and breathing circuit). Exhaled gas is sampled by a dedicated analyser (anaesthetic monitor or some defibrillators).
Typically such methods generate both a waveform (capnograph) and a number (ETCO2).
The normal capnograph trace can be divided into distinct phases
I – the end of inspiration & the beginning of expiration, when the Co2-free gas occupying dead space in airway is exhaled. Hence in theis phase the ETCO2 = 0 mmHg
II – there is a rapid rise in measured CO2 as alveolar gas appears
III – expiration continues but CO2 doesn’t rise much further – a plateau in normal lungs. ETCO2 total is derived from the maximum on this plateau
IV – a sharp drop in CO2 to zero, representing inspiration
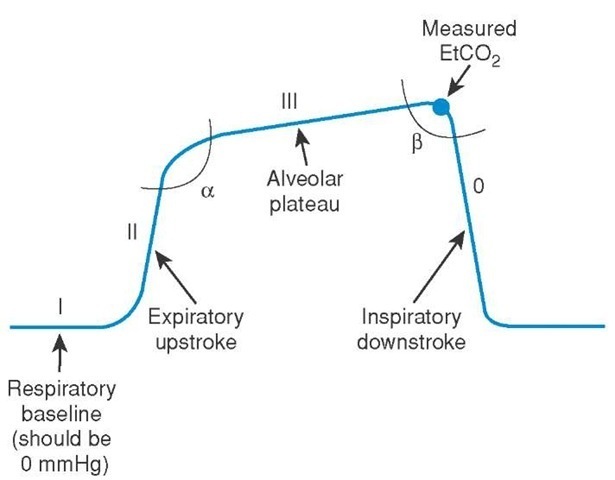
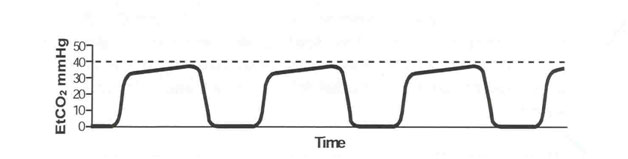
The capnograph gives us lots of information in addition to the absolute number of ETCO2 (aim 35-45 mmHg). It is easiest to consider the waveform baseline, height, frequency, rhythm & shape.
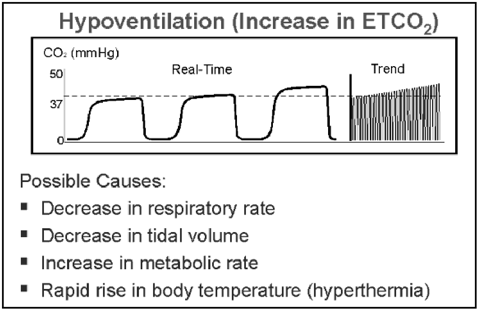
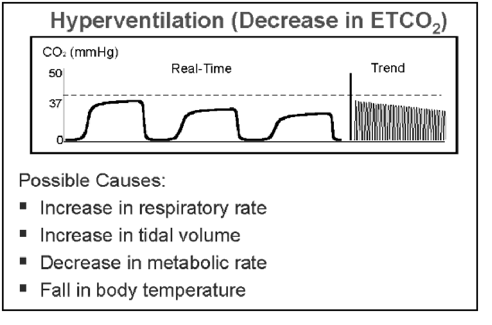
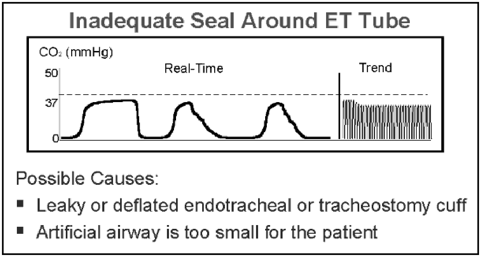
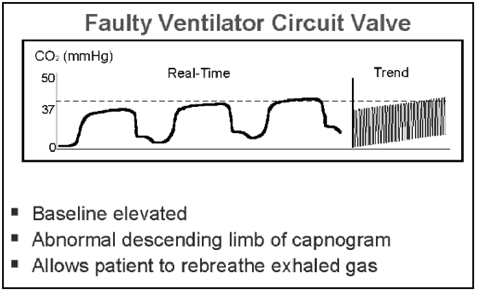
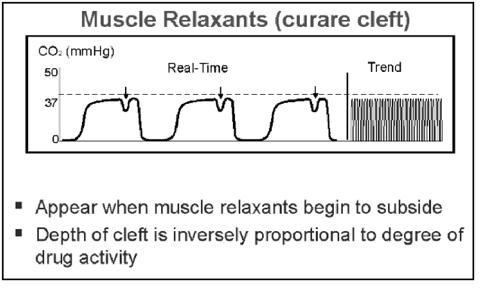
You can correlate changes in patient or equipment as being reflected in the ETCO2 trace eg:
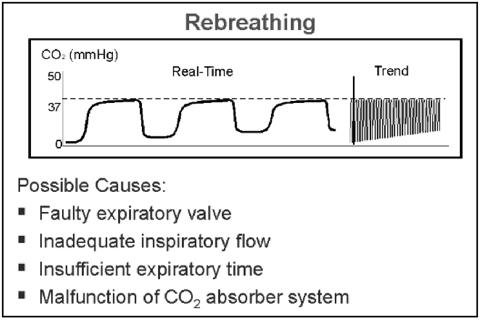
baseline – non-return to zero caused by re-breathing
height – increasing ETCO2 due to excess production eg: malignant hyperthermia
frequency – decrease or increase in ETCO2 peaks in hypo- and hyperventilation respectively
rhythm – patient breathing vs mechanical ventilation as neuromuscular blockade wears off
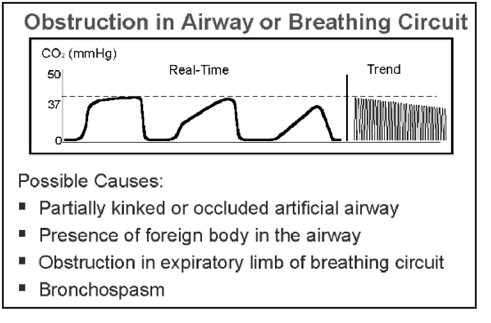
shape – obstructive ventilation pattern causes a slow phase II upstroke
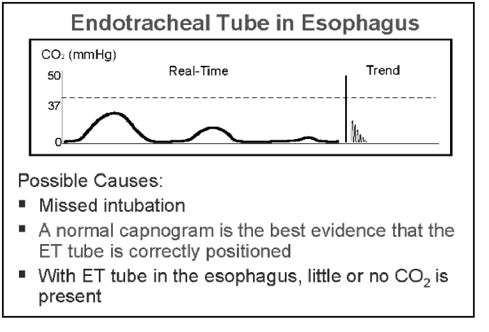
There are some must know waveforms in the ‘rogues gallery’ later below. The ones I worry about most are the absent or rapidly disappearing ETCO2 rtace seen in inadvertent oesophageal intubation…and the falling ETCO2 waveform with loss of cardiac output.
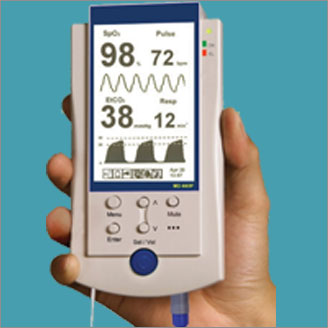
(iii) waveform capnography – during spontaneous ventilation
As an alternative to sampling expired gas directly from the anaesthetic circuit or HME filter attached to an endotracheal tube, it may be useful to monitor ETCO2 for spontaneously ventilating patients, whether on room air, nasal specs or oxygen mask.
I use this routinely during endoscopy, colonoscopy in the operating theatre, as well as when performing procedural sedation in the ED. I am increasingly using ETCO2 monitoring to confirm ventilation in other situations – particularly to confirm ongoing ventilation of the agitated psychiatric patient who has been effectively sedated with agents such as benzodiazepines, haloperidol or ketamine – mindful that hypoventilation or apnoea may be missed.
Remember that relying on SpO2 to confirm ventilation is inadequate – measured oxygen saturation may remain elevated for some time after cessation of breathing- and once a fall in SpO2 has been detected, your patient is already hurtling down the oxy-haemo-coaster.
Beware the falsely reassuring statement “He must be breathing – the sats are OK” – use ETCO2 to gauge ventilation
In ED ot theatre, there are different gizmos. Most ETCO2 sampling equipment is dedicated to sit in-line as either an adaptor between ETT and circuit, or as a filter line to attach to HME filter. There are also sampling devices designed to sit under nares like nasal specs.
I tend to just take the sampling line from the HME filter, attach to a microfilter and then attach to either blunt cannula or plastic tube of an IV – this can be pushed through the holes in a Hudson mask to detect ETCo2 for patients receiving sedation NB: the ETCo2 will be LOW as diluted by oxygen.
Ubiquitous Dr Minh le Cong offers some hints on MacGyvering ETCO2 setups below :
Prehospitalmed.com “Capnography with LifePak 15” – Dr Minh le Cong
Noninvasive Capnography Setup (PK talk) – Dr Minh le Cong
as do the mob from the EM resource ‘Standing on the corner minding own business’ (SOCMOB)
“how to make your own end-tidal CO2 detector“
When should I measure ETCO2?
End-tidal CO2 is classically considered as the standard of care when performing intubation. Either colorimetric or waveform capnography can be used to confirm the presence of exhaled CO2 and hence confirm desired tracheal vs inadvertent oesophageal intubation.
The waveform also gives clues to alveolar ventilation (hypo- or hyperventilation), airway resistance, cardiac output, CO2 production & elimination, as well as the obvious confirmation of tube placement within the trachea – both initial & ongoing.
Other uses include :
- confirmation of tube placement & efficiency of compressions during CPR
- sudden increase in ETCO2 during CPR may indicate ROSC
- during sedation to confirm ventilation when direct observation of the patient may be difficult (eg: under drapes/blankets/on side)
- in psychiatric sedation to achieve effective sedation & avoid apnoea
- during transfer to confirm presence of cardiac output & adequate ventilation
- as a numeric target to aim for eg: in treating the head-injured patient where normocarbia, normotension and avoidance of hypoxia are key goals to avoiding rises in ICP.
Thus we can summarise ETCO2 measurement as :
- to confirm tube placement
- to confirm ventilation & perfusion of patients during mechanical ventilation
- to confirm ventilation of patients who SHOULD be self-ventilating (but at risk of hypopnoea or apnoea)
The clinical bottomline?
End-tidal CO2 monitoring is mandatory not just for the intubated patient, but should be used whenever using a neurolept eg: sedation in ED, monitoring of psychiatric patient etc.
Even if you are not performing anaesthesia, know how to hook up ETCO2 monitoring for your spontaneously ventilating patients at risk of hypopnoea or apnoea.
Dedicated ETCO2 monitors exist, but most capnographs will hook up to existing monitors in OT, ED and ward defibs.
Insist on the use of ETCO2 monitoring in your shop.

Where can I find out more?
Life in the Fast Lane posts on capnography and interpreting waveforms
Check out Prof Kodali’s website capnography.com & read his excellent paper entitled “Capnography outside operating rooms” (download here)
You may also be interested to read those Norse Gods of resus (ScanCrit) on capnography in cardiac arrest & Cliff Reid’s post on ‘even the dead exhale CO2’ – explaining why you MUST use waveform capnography in resus
ROGUES GALLERY OF ‘MUST KNOW’ ETCO2 WAVEFORMS
NB: these images downloaded from Google. I haven’t been able to find the author to attribute, so apologies if unattributed. I reckon an American source (who else omits the diphthong in oesophagus?)
SUMMARY OF CAUSES & ETCO2 CHANGES
FLAT ETCO2 TRACE
- Capnograph not connected
- Oesophageal intubation
- Airway (ETT) misplaced
- Respiratory or cardiac arrest
- Capnograph sampling tube kinked or blocked
- No ventilation – either forgot to bag the patient or there is a ventilator malfunction
SUDDEN DROP IN ETCO2 TO ZERO
- Kinked ET tube
- CO2 analyzer defective
- Total disconnection
- Ventilator defective
SUDDEN CHANGE IN BASELINE (NOT TO ZERO)
- Calibration error
- CO2 absorber saturated (check capnograph with room air)
- Water drops in analyser or condensation in airway adapter
SUDDEN INCREASE IN ETCO2
- ROSC during cardiac arrest
- Correction of ET tube obstruction
ELEVATED INSPIRATORY BASELINE
- CO2 rebreathing (e.g. soda lime exhaustion)
- Contamination of CO2 monitor (sudden elevation of base line and top line)
- Inspiratory valve malfunction
INCREASED ETCO2
CO2 production
- Fever
- Sodium bicarbonate
- Tourniquet release
- Venous CO2 embolism
- Overfeeding
Pulmonary perfusion
- Increased cardiac output
- Increased blood pressure
Alveolar ventilation
- Hypoventilation
- Bronchial intubation
- Partial airway obstruction
- Rebreathing
Apparatus malfunction
- Exhausted CO2 absorber
- Inadequate fresh gas flows
- Leaks in ventilator tubing
- Ventilator malfunctioning
DECREASED ETCO2
CO2 production
- Hypothermia
Pulmonary perfusion
- Hypotension
- Hypovolemia
- Pulmonary embolism
- Reduced cardiac output
- Cardiac arrest
Alveolar ventilation
- Hyperventilation
- Apnea
- Total airway obstruction (high airway pressures)
- Extubation
Apparatus malfunction
- Circuit disconnection (low airway pressures)
- Leaks in sampling tube
- Ventilator malfunctioning


Pingback: The LITFL Review 118 - LITFL
Wow, great article! Thanks Tim. During training of students and residents, I make it clear to them that the waveform size and shape tells us how well they are ventilating.
A nice easy to understand article. Thanks for this KI Doc
What I want to understand more clearly is why the intubated patients waveform changes shape when mechanically ventilated vs spontaneously ventilating. Also why does the inspiratory slope decrease with inspiratory valve malfunction, but only the baseline increases with expiratory valve malfunction. All sources I have found simply state that “this is how the waveform changes in this instance” but does not explain why??
Thanks!!
Pingback: Funtabulously Frivolous Friday Five 269 • LITFL